Erin Saricilar, Raleene Gatmaitan, Kiraati Patel, Mark Yang
|
Abstract Atherosclerotic disease significantly impacts patients with type 2 diabetes, who often present with recalcitrant peripheral ulcers. The angiosome model of the foot presents an opportunity to perform direct angiosome-targeted endovascular interventions to maximise both wound healing and limb salvage. A systematic review was performed, with 17 studies included in the final review. Below-the-knee endovascular interventions present significant technical challenges, with technical success depending on the length of lesion being treated and the number of angiosomes that require treatment. Wound healing was significantly improved with direct angiosome-targeted angioplasty, as was limb salvage, with a significant increase in survival without major amputation. Indirect angioplasty, where the intervention is applied to collateral vessels to the angiosomes, yielded similar results to direct angiosome-targeted angioplasty. Applying the angiosome model of the foot in direct angiosome-targeted angioplasty improves outcomes for patients with recalcitrant diabetic foot ulcers in terms of primary wound healing, mean time for complete wound healing and major amputation-free survival. Keywords: Diabetic foot ulcer, angiosome, angioplasty Disclosure: The authors have no conflicts of interest to declare. Received: Accepted: Published online: Citation:Vascular & Endovascular Review 2023;6:e04. DOI: https://doi.org/10.15420/ver.2022.08 Acknowledgements:The authors thank Royal North Shore Hospital for providing support for this research project. Open Access: This work is open access under the CC-BY-NC 4.0 License which allows users to copy, redistribute and make derivative works for non-commercial purposes, provided the original work is cited correctly. |
Open bypass, while the gold standard in iliofemoral disease, remains challenging in microvascular disease; therefore, there is a significant, increasing and enduring role for minimally invasive endovascular surgery as first-line treatment.1
Patients with diabetes have increased risk of developing chronic ulceration in pressure areas of their extremities due to a multitude of factors including increased microvascular atherosclerotic changes, as well as a weakened immune system, particularly when the diabetes is uncontrolled.2,3
Major amputation is a procedure with high morbidity, with perioperative mortality in below-knee amputation at 8–10% and above-knee amputation at 15–20%. Furthermore, 2-year mortality after a major amputation is 40%, with a second amputation being necessary in 30% of cases.4,5 With further amputations, larger prostheses are needed to maintain function, which require increased cardiac output in patients with poor cardiorespiratory reserve.
The angiosome concept was initially described by Taylor and Palmer in their 1987 study; this divides the human body into 3D regions supplied by individual distal arteries and drained by individual veins.6 This concept has since been extensively used in the field of plastic surgery where careful isolation and delineation of vascularised regions of the body are paramount.
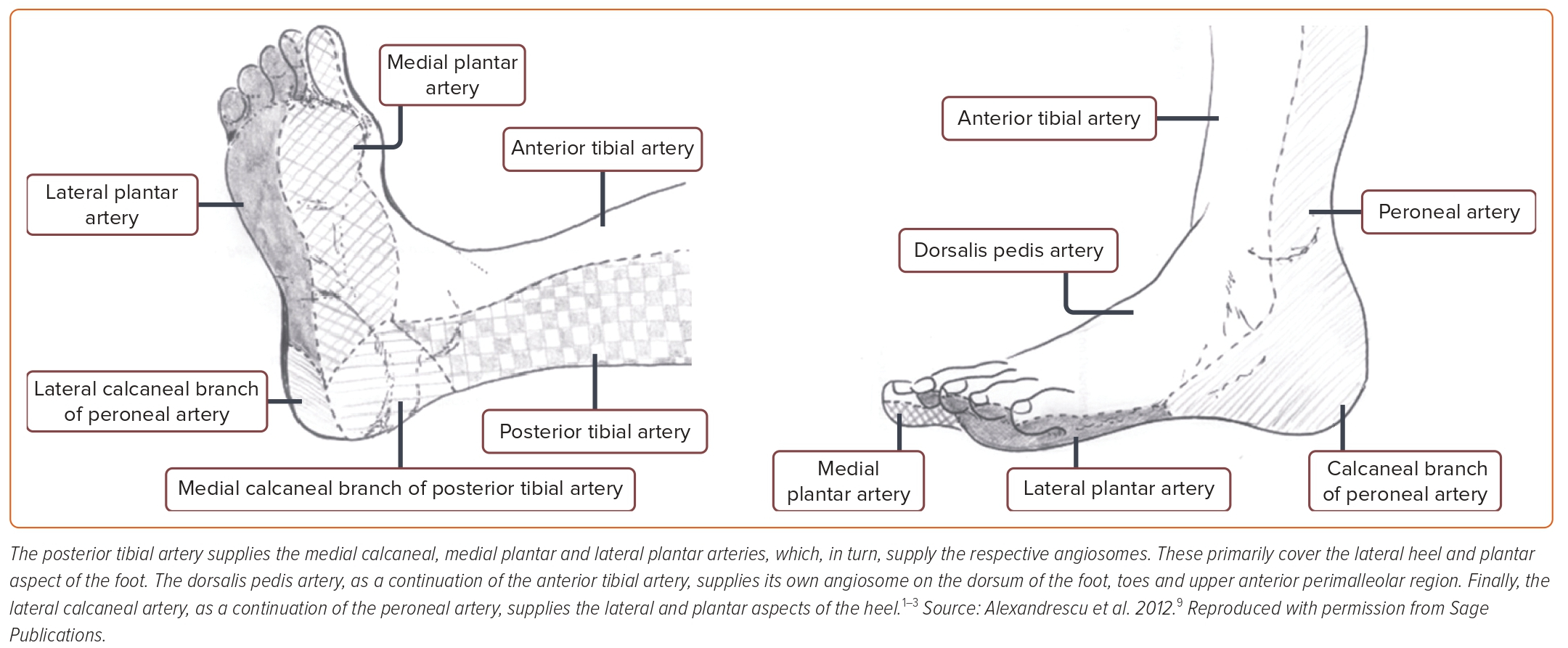
Figure 1: Artery Supply
Attinger et al. extended the angiosome concept categorically to the foot by dividing it into six angiosomal regions, each supplied by one of the three crural arteries (Figure 1).7 This opened the doors theoretically to the ability to treat ulcerated regions of a limb selectively by isolating the feeding arteries through a method called direct angiosome-targeted angioplasty.8,9 Prioritising inline flow to the relevant angiosome and avoiding unnecessary risk to indirect blood vessels, in theory, would benefit the overall care of the patient.
The goal of this systematic review was to explore the evidence around the use of direct angiosome-targeted angioplasty to treat diabetic foot ulcers and to broadly summarise findings. The following research questions will be answered in the PICOS (population, intervention, comparison, outcomes and study) format:
- Is direct angiosome-targeted angioplasty safe to use in patients with diabetes who have foot ulcers?
- Is there any added benefit to using direct angiosome-targeted angioplasty on patients with diabetes who have foot ulcers when evaluating wound healing and limb salvage?
Methods
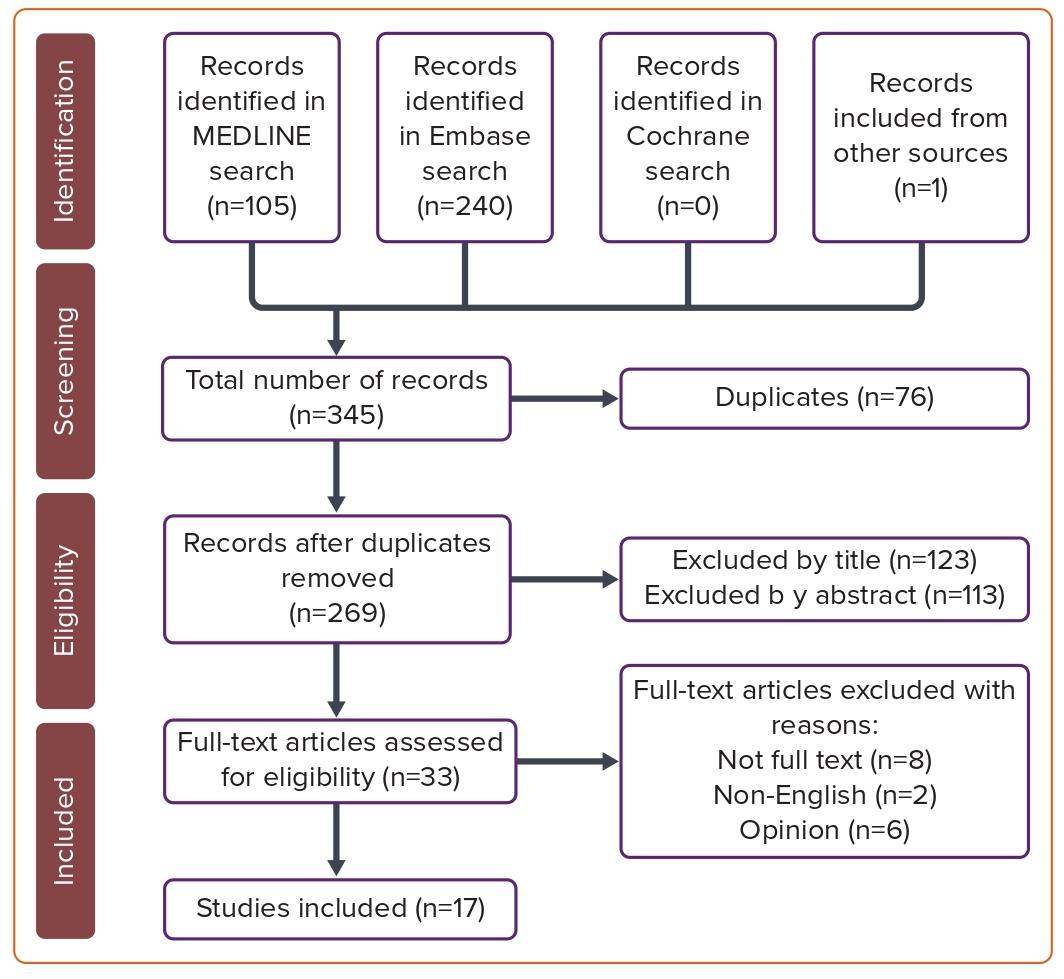
A systematic review was performed using the protocols set out by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, which describe the minimum required reporting in a systematic review. The steps followed are summarised in a PRISMA flow diagram (Figure 2).10
Figure 2: PRISMA Diagram
Criteria for Selecting Studies for this Review
A search strategy was used (Supplementary Material Table 1). Inclusion and exclusion criteria were implemented based on definitions developed by the EQUATOR network, which is a group dedicated to developing high-quality research guidelines (Supplementary Material Table 2).10
The population arm focused on patients with diabetic foot ulcers, while the intervention was endovascular treatment. While a control was not included in the search, the comparison intervention was angioplasty and endovascular treatment. The outcomes focused on survival, mortality, complications, wound healing and limb salvage. These terms were broad and narrowed down in the title, abstract and full-text reviews. All MeSH terms were exploded and included in the search.
There was extensive exclusion because of article design, definitions, interventions, cohort, protocol and statistics through a title and abstract review. Articles where only the abstract was available and those that were not in English as well as opinion articles were excluded. Specific to the definition of terms in the research question, articles that mentioned the angiosome model but did not directly study it were not included. For each article, an intervention/treatment measure that was repeatable and well defined had to be evaluated and statistical significance calculated using a reproducible and well-described statistical method; however, in the initial screening, the validity of the method was not considered. All research included needed to be published in a peer-reviewed journal and not redacted.
Search Methods to Identify Studies
A search of Ovid MEDLINE from 1946, Embase Classic and Embase since 1947 and all Cochrane Reviews to 21 February 2021 was carried out.
Data Collection and Analysis
All of the results from each of the database searches were imported into EndNote (Clarivate) and duplicates merged or removed. The titles, followed by the abstracts, were all independently evaluated by authors ES and RG. Two selection rounds were then used to select the final articles for inclusion, with any discrepancies independently evaluated by MY and then either included or excluded from the study. Data were extracted from the reports by ES and the final completed tables were evaluated by MY and JN for appropriateness and thoroughness.
The data items that were extracted included:
- study type;
- funding;
- population;
- sample size;
- intervention;
- control (if any);
- outcomes; and
- statistical analysis used and significance (if any).
These data items are summarised in Supplementary Material Table 3. Relevant to the systematic review, the prioritised outcomes included the population with sample size, the intervention and the outcomes. All statistical analysis of the quantitative data was performed using SPSS version 26 (IBM Corporation) and Excel 2019 (Microsoft).
Qualitative results are summarised in Supplementary Materials Table 4 and are evaluated within the discussion of this systematic review, albeit with the acknowledgement that they are likely to provide lower-quality evidence.
The risk of bias in the included studies was assessed based on the MOOSE criteria, which were developed by the EQUATOR network.11 It strives to develop a set of criteria for assessing risk in observation and non- randomised cohort studies, which make up the vast majority of results for this research question and search strategy. The reported methods and protocols were assessed for relevance, reproducibility, consideration of risks of bias, statistical methods and appropriate reporting.
The information is tabulated using the Oxford Centre for Evidence-Based Medicine levels of evidence (Supplementary Table 3).12 The confidence in cumulative evidence was based on the GRADE approach.13–15 Five key criteria were used to assess the potential for lower-quality evidence.
The design and implementation of the study were investigated to identify limitations that may lead to bias. If the evidence was indirect within the PICOS format, this was considered to reduce confidence in it. Concurrently, an unexplained heterogeneity of results showed potential bias. Wide confidence intervals also suggested imprecision in results. Finally, the probability of publication bias was assessed.
The involvement of all authors is summarised in Supplementary Material Table 5.
Results
The search strategy yielded 269 articles, of which 236 were excluded for various reasons (Supplementary Material Table 2). This left 33 articles for full assessment, of which eight were without full text, two non-English and six opinion articles were excluded. Finally, 17 articles were included in this study.
Articles with level 1–3 evidence based on the Oxford 2011 Levels of Evidence guidelines with quantitative data are summarised in Supplementary Material Table 3, while those with qualitative data are summarised in Supplementary Material Table 4.12
Discussion
Traditionally, open bypass surgery has been the gold standard treatment for critically ischaemic limbs by bypassing the lesion completely. However, with the growing advent of highly specialised endovascular techniques, the use of endovascular interventions is recommended in high-risk patients and as initial intervention, presenting similar outcome results as open bypass.4,16
The angiosome model, when initially described specifically for vascular surgery and diabetic foot ulcers, was not supported by enough longitudinal data to recommend it, although in theory it could help guide vessel selection, vascular access and specific strategies.9 As all intimal injury can lead to significant issues, minimising intervention and limiting handling to only areas that require management could be justified in principle.9,17
As patients with diabetes have a different profile of vascular disease from those without the condition, notably with microvascular disease and compromised immune response, the role of direct angiosome-targeted angioplasty needs to be compared between the two classes of patients. Fortunately, no significant difference has been demonstrated between patients with and without diabetes when considering limb salvage at 1 year follow-up, regardless of angiosome-directed intervention.18
Technical Challenges
Endovascular interventions can be technically difficult in infra-popliteal vessels, particularly where atherosclerotic disease is present in the crural vessels. Crossing the lesion, creating clinically relevant revascularisation and avoiding rupture all need to be considered in any endovascular intervention.
In most studies included in this review, technical success ranged between 60.9 and 84.7%.4,8,19 This is in contrast to a meta-analysis of infra-popliteal angioplasty, notably of the popliteal vessel and tibioperoneal trunk, which demonstrated a pooled technical success of 89.0%.20
It becomes apparent that, while significant challenges present in directly treating angiosomes, some studies reported an ability to achieve technical success close to that of traditional infra-popliteal angioplasty. The only factor negatively impacting on procedure’s technical difficulty was an increase in the length of the occlusion being treated.19 Lesion distribution can compound this and can compromise a successful outcome, particularly in the crural vessels. With multiple lesions throughout a single angiosome-supplying artery, the procedure becomes increasingly difficult technically, which may present as a limiting factor in achieving success.
Technical difficulty increases with the number of angiosome-specific vessels that require treatment. Spillerova et al. determined the impact of the number of interventional vessels on technical success and reported a significant plummet in success at four angiosomes to 25%, and no possibility of revascularisation where more than five angiosomes were involved.8 In context, treating one, two and three angiosomes had high levels of success (69.2, 86.7 and 85.7%, respectively), with overall technical success being 60.9%.8
Potentially compromising the ability to directly treat angiosomes are anatomical variations, which are common within the general population. Type III branching from the popliteal artery was the most common variant (1.0–7.6%), which risks poor distal supply with hypoplastic or aplastic crural vessels: posterior tibial artery (0.8–5.1%), anterior tibial artery (0.1–1.7%) and both posterior and anterior tibial arteries (0.1–0.8%).21,22 Correlating with these both angiographic and cadaveric findings, 6.5% of infrapopliteal arterial anatomical variants were found in 6.5% of patients with chronic Rutherford category 5 and 6 chronic ischaemia requiring lower limb salvage interventions, with 4.8% being type III variants.22
Clinical Outcomes
The success of a procedure clinically can be technically defined by the oxygen tension (TcPO2) value, with direct angiosome-targeted angioplasty significantly improving TcPO2.17,23 Additionally, ankle-brachial indices improved concurrently and at statistically significant levels.23 This demonstrates that even limited angioplasty using an angiosome model can deliver significantly better technical results, not considering the clinical outcomes of the interventions performed.
From a more clinical setting, there was considerable heterogeneity between studies when investigating healing rates. Chae and Shin performed a meta-analysis on four studies demonstrating a significant improvement in healing rate though, unfortunately, not correcting for follow-up time.24 Delving into the studies included in the meta-analysis, no significant difference was noted between single-vessel and multiple-vessel revascularisation.25
Factors that correlate with negative outcomes include Wagner grade 3–4 lesions, a patient being confined to bed for the long term, left ventricular dysfunction, end-stage renal disease and peripheral neuropathy, the latter two being common in those with diabetes.26 All these factors need to be considered when intervening on patients with multiple comorbidities. Regardless, however, these patients benefit from direct angiosome- targeted angioplasty, with better wound healing demonstrated when this is performed regardless of the number of vessels remaining patent after the procedure.9,26,27
Across the vast majority of studies investigating direct and indirect revascularisation, significantly improved healing rates were demonstrated.16,28,29 Additionally, when adjusting for propensity score, the direct angiosome-targeted cohort had better wound healing rates.30 In the largest cohort of patients with type 2 diabetes, in a study by Iacopi et al. that recruited 603 patients, significant improvements in healing rates as well as mortality were demonstrated with both direct and indirect angioplasty.28 Notably, Fossaceca et al.’s study did not demonstrate a significant difference between direct and indirect angiosome-targeted angioplasty when assessing for wound healing, but still recommended direct intervention as first-line therapy.28,31 When included in a broader meta-analysis, it supported the use of direct angiosome-targeted angioplasty to improve wound healing.24
The study by Alexandrescu et al. was the only prospective multicentre longitudinal study. Direct angiosome-targeted angioplasty for revascularisation demonstrated improvements in wound healing (p=0.011) and mean time to heal (p=0.001).29 With a cohort of 167 patients with diabetes, this was a broad study with strong methodology that supports direct revascularisation techniques.
Limb Salvage
Limb salvage concerns the period when a patient is free from major amputation. The vast majority of studies that demonstrated wound healing similarly showed improved limb salvage rates. Early studies with direct angiosome-targeted angioplasty resulted in 5.2% of patients requiring above-the-ankle amputations.23 Similarly, limb salvage rates of between 68.8% and 93% within 12 months were achieved across the vast majority of studies.4,17,19
Freedom from amputation as limb salvage improved, based on the angiosome model in a retrospective model, which was also demonstrated in a similar prospective study.27,29 A meta-analysis demonstrated a significant improvement in limb salvage rates when direct angiosome-targeted angioplasty was performed (p<0.001).24 Thirty-day freedom from major amputation was seldom described in the research, but was as low as 2%.25
Collateralisation
A contrasting model of treatment investigates the role of collateralisation in wound healing. In patients with chronic limb ischaemia, it is known that angiogenesis promotes collateral vessels providing nutrients to distal portions of the limbs. Flow into these collateral vessels can be restricted by disease.
A recent systematic review demonstrated that direct angiosome-targeted angioplasty has similar outcomes to indirect revascularisation via collateral vessels.32 At the 24 months mark in one series of 76 patients, there were similar results between these two groups in limb salvage at 93% versus 88% (p=0.59) and mean ulcer healing at 12 months of 92% versus 85% (p=0.12).16 Another series with 92 patients yielded similar results, with a 24-month limb salvage rate of 89% versus 85%, and 12-month wound healing at 66% versus 68%.25
A comparison of indirect revascularisation via collateral vessels with indirect revascularisation without collateral vessels showed significantly better healing and limb salvage rates in the former.18
Revision Rates
With patients being at high risk of intimal hyperplasia, the success of angioplasty can often be measured by revision rates. Unfortunately, none of the studies included evaluated the role of drug-coated balloons, which is a controversial topic in itself, and statements were rarely made about whether a plain balloon had been used. Accordingly, judgements cannot be made on the effects of types of angioplasty balloons.
However, a meta-analysis of four studies demonstrated no significant difference in revision rates between direct angiosome-targeted angioplasty and indirect angioplasty (p=0.314).24
Limitations
While many of the studies included had strong methodology, the vast majority were retrospective case series or longitudinal observational cohort studies. Only one prospective study and no randomised controlled trials were included, which makes it challenging to draw definitive conclusions from the data presented. Additionally, a single meta-analysis had a limited number of studies included, albeit very well performed.
A well-defined and comprehensive randomised controlled trial would be beneficial and ethical to better guide endovascular treatment of recalcitrant diabetic foot ulcers.
Conclusion
Even with a lack of randomised controlled trials, there is significant evidence to support the use of direct angiosome-targeted angioplasty to treat recalcitrant diabetic foot ulcers as both safe and efficacious. Compared to indirect angioplasty, it leads to wound healing, limb salvage and mortality benefits, albeit no difference in revision rates.
There is also considerable evidence to consider treatment of collateral vessels that may not have direct perfusion capacity based on the angiosome model.
Click here to view Supplementary Material
- Norgren L, Hiatt WR, Dormandy JA, et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg 2007;45(Suppl):S5–S67.
Crossref | PubMed - Lee KM, Kim WH, Lee JH, Choi MSS. Risk factors of treatment failure in diabetic foot ulcer patients. Arch Plast Surg 2013;40:123–8.
Crossref | PubMed - Prompers L, Huijberts M, Apelqvist J, et al. High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia 2007;50:18–25.
Crossre |PubMed - Dayananda L, Moorthy S, Sreekumar K, et al. Infrapopliteal angioplasties for limb salvage in diabetic patients: does the clinical outcome justify its use? Indian J Rad Imaging 2008;18:156–61.
Crossref - Bal A, Das A, Pendsey S, et al. Handbook of diabetic foot care. Bangalore, India: Diabetic Foot Society of India, 2005.
- Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg 1987;40:113–41.
Crossref | PubMed - Attinger CE, Evans KK, Bulan E, et al. Angiosomes of the foot and ankle and clinical implications for limb salvage: reconstruction, incisions, and revascularization. Plast Reconstr Surg 2006;117(7 Suppl):261S–93S.
Crossref | PubMed - Spillerova K, Sorderstrom M, Alback A, Venermo M. The feasibility of angiosome-targeted endovascular treatment in patients with critical limb ischemia and foot ulcer. Ann Vasc Surg 2016;30:270–6.
Crossref | PubMed - Alexandrescu V, Soderstrom M, Venermo M. Angiosome theory: fact or fiction? Scand J Surg 2012;101:125–31.
Crossref | PubMed - Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta–analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12.
Crossref | PubMed - Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008–12.
Crossref | PubMed - Oxford Centre for Evidence-Based Medicine Levels of Evidence Working Group. The Oxford Levels of Evidence. 2011 (accessed 27 March 2023).
- Schünemann HJ, Higgins JPT, Vist GE, et al. Chapter 14. Completing ‘summary of findings’ tables and grading the certainty of the evidence. In: Higgins JPT, Thomas J, Chandler J, et al., eds. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK: John Wiley & Sons, 2019;375–402.
Crossref - Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401–6.
Crossref | PubMed - Schünemann HJ, Cuello C, Akl EA, et al. GRADE guidelines: 18. How Robins-I and other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence. J Clin Epidemiol 2019;111:105–14.
Crossre |PubMed - Varela C, Acin F, de Haro J, et al. The role of foot collateral vessels on ulcer healing and limb salvage after successful endovascular and surgical distal procedures according to an angiosome model. Vasc Endovasc Surg 2010;44:654–60.
Crossref | PubMed - Ferraresi R, Centola M, Ferlini M, et al. Long-term outcomes after angioplasty of isolated, below-the-knee arteries in diabetic patients with critical limb ischaemia. Eur J Vasc Endovasc Surg 2009;37:336–42.
Crossref | PubMed - Zheng XT, Zeng RC, Huang JY, et al. The use of the angiosome concept for treating infrapopliteal critical limb ischemia through interventional therapy and determining the clinical significance of collateral vessels. Ann Vasc Surg 2016;32:41–9.
Crossref | PubMed - Cildag MB, Koseoglu OFK, Ertugrul MB. Infrapopliteal percutan transluminal angioplasty of patients with TASC D group diabetic foot lesions according to the transatlantic inter-society consensus II. Med Bull Haseki 2017;55:125–30 [in Turkish].
Crossref - Romiti M, Albers M, Brochado-Neto FC, et al. Meta-analysis of infrapopliteal angioplasty for chronic critical limb ischemia. J Vasc Surg 2008;47:975–81.
Crossref | PubMed - Kim D, Orron DE, Skillman JJ. Surgical significance of popliteal arterial variants. A unified angiographic classification. Ann Surg 1989;210:776–81.
Crossref | PubMed - Kawarada O, Yokoi Y, Honda Y, Fitzgerald PJ. Awareness of anatomical variations for infrapopliteral intervention. Catheter Cardiovasc Interv 2010;76:888–94.
Crossref | PubMed - Faglia E, Mantero M, Caminiti M, et al. Extensive use of peripheral angioplasty, particularly infrapopliteal, in the treatment of ischaemic diabetic foot ulcers: clinical results of a multicentric study of 221 consecutive diabetic subjects. J Intern Med 2002;252:225–32.
Crossref | PubMed - Chae KJ, Shin JY. Is angiosome-targeted angioplasty effective for limb salvage and wound healing in diabetic foot?: a meta-analysis. Plos One 2016;11:1–11.
Crossref | PubMed - Acín F, Varela C, López de Maturana I, et al. Results of infrapopliteal endovascular procedures performed in diabetic patients with critical limb ischemia and tissue loss from the perspective of an angiosome-oriented revascularization strategy. Int J Vasc Med 2014;2014:1–13.
Crossref | PubMed - Alexandrescu VA, Hubermont G, Philips Y, et al. Selective primary angioplasty following an angiosome model of reperfusion in the treatment of Wagner 1–4 diabetic foot lesions: practice in a multidisciplinary diabetic limb service. J Endovasc Ther 2008;15:580–93.
Crossref | PubMed - Alexandrescu V, Vincent G, Azdad K, et al. A reliable approach to diabetic neuroischemic foot wounds: below-the-knee angiosome-oriented angioplasty. J Endovasc Ther 2011;18:376–87.
Crossre |PubMed - Iacopi E, Coppelli A, Goretti C, et al. Effect of direct endovascular revascularization based on the angiosome model on risk of major amputations and life expectancy in type 2 diabetic patients with critical limb ischemia and foot ulceration. J Am Podiatr Med Assoc 2021;111:18-130.
Crossref | PubMed - Alexandrescu VA, Brochier S, Limgba A, et al. Healing of diabetic neuroischemic foot wounds with vs without wound-targeted revascularization: preliminary observations from an 8-year prospective dual-center registry. J Endovasc Ther 2020;27:20–30.
Crossref | PubMed - Soderstrom M, Alback A, Biancari F, et al. Angiosome-targeted infrapopliteal endovascular revascularization for treatment of diabetic foot ulcers. J Vasc Surg 2013;57:427–35.
Crossref | PubMed - Fossaceca R, Guzzardi G, Cerini P, et al. Endovascular treatment of diabetic foot in a selected population of patients with below-the-knee disease: is the angiosome model effective? Cardiovasc Intervent Rad 2013;36:637–44.
Crossre |PubMed - Forsythe RO, Apelqvist J, Boyko EJ, et al. Effectiveness of revascularisation of the ulcerated foot in patients with diabetes and peripheral artery disease: a systematic review. Diabetes Metab Res Rev 2020;36(Suppl 1):1-9.
Crossref | PubMed