Stavros Spiliopoulos, Lazaros Reppas, Konstantinos Palialexis, Elias Brountzos
|
Abstract Over 20 million adults in Europe suffer from peripheral arterial disease (PAD). The annual incidence of PAD is approximately 2.4%, while the annual incidence of critical limb ischaemia (CLI), the last and most severe stage of PAD, has been reported to be 0.4%. Endovascular angioplasty and/or stenting of infrapopliteal disease is, today, an established treatment for critical limb ischaemia. The main technical advantages of endovascular treatment over open bypass surgery include the possibility to revascularise more than one infrapopliteal vessels and, most importantly, to treat outflow pedal vessel disease or even reconstitute the pedal arch. Data of below-the-ankle angioplasty are beginning to sum up and the contribution of pedal arch angioplasty in limb salvage and wound healing are currently under investigation. In this review, currently available data and the future perspectives on below-the-ankle and pedal arch endovascular treatment will be presented. Keywords Critical limb ischaemia, balloon angioplasty, wound healing, amputation, endovascular treatment, pedal arch angioplasty. Disclosure: The authors have no conflicts of interest to declare; Received: Accepted: Published online: Citation: Vascular & Endovascular Review 2019:2(1):6–8.; DOI: https://doi.org/10.15420/ver.2018.19.2 Correspondence Details: Stavros Spiliopoulos, 2nd Radiology Department, Interventional Radiology Unit, University of Athens, Attikon University General Hospital, Athens, Greece. Email: stavspiliop@med.uoa.gr Open Access:
This work is open access under the CC-BY-NC 4.0 License which allows users to copy, redistribute and make derivative works for non-commercial purposes, provided the original work is cited correctly. |
More than 20 million adults in Europe have peripheral arterial disease (PAD) and the worldwide prevalence of the disease increases to 20% for patients over 70 years of age.1 The annual incidence of PAD is approximately 2.4%, while the annual incidence of critical limb ischaemia (CLI), the last and most severe stage of PAD, has been reported to be 0.4%.2 CLI is a limb-threatening pathology that has been correlated with exceedingly high amputation rates when prompt revascularisation is not offered. A mortality rate of over 50% at 5 years after the diagnosis has been reported.3,4
The goal of revascularisation is the establishment of adequate reperfusion of the foot tissue to relieve ischaemic symptoms and enable wound healing, which is usually achieved by creating a straight line of blood flow to the distal foot. Patients with CLI usually present with multilevel vascular disease involving the iliac, femoropopliteal and infrapopliteal vessels. However, in CLI patients with comorbidities, such as diabetes or end-stage renal disease (or both), the involvement of infrapopliteal and pedal arch disease is characteristic and frequent.5
Endovascular angioplasty and/or stenting of infrapopliteal disease is an established treatment for CLI. The main reasons why distal bypass surgery is either not recommended or frequently not feasible include high surgical risk of the patient, unavailability of an autologous venous conduit, poor-quality arterial runoff and extensive pedal arch disease.6,7 In contrast, minimally invasive infrapopliteal angioplasty and stenting does not necessitate general anaesthesia, requires less procedural time than open bypass surgery, results in low complication rates and can be easily repeated. Furthermore, the main technical advantages of endovascular treatment over open bypass surgery include the option to revascularise more than one infrapopliteal vessel and, most importantly, to treat outflow pedal vessel disease or even reconstitute the pedal arch.
It was nearly 20 years ago when endovascular pioneers published the first data on infrapopliteal balloon angioplasty and stenting, paving the way towards more effective endovascular treatment of CLI.8-10 With the advent of novel, improved, dedicated infrapopliteal endovascular devices such as 0.014-inch guidewires and supporting catheters, as well as tapered, low-profile, angioplasty balloon catheters, the possibility of safe and feasible below-the-ankle and pedal arch vessel angioplasty has arisen.
Moreover, the development of retrograde pedal arterial access using dedicated low-profile sheaths and novel revascularisation techniques including the subintimal arterial flossing with antegrade-retrograde intervention (SAFARI) dual access technique, have broadened the indications and further improved the success rates of previously technically impossible endovascular procedures.11
Data So Far
The first study to compare below-the-knee angioplasty with or without pedal arch angioplasty was published in 2009 by Manzi et al.11 This study employed the pedal-plantar loop technique first described in a case report by Fusaro et al. in 2007.12 Manzi et al. investigated 135 consecutive CLI patients treated with the pedal-plantar loop technique in a prospectively maintained registry. These patients were compared with a retrospectively analysed cohort of 1,331 CLI patients who underwent below-the-knee angioplasty only. Acute technical success in the pedal-plantar loop group was 85%, compared with 100% in the below-the-knee angioplasty group. The 1-year limb salvage rate was similar between the two groups. However, at the 15-day follow-up, a significant improvement in transcutaneous oxygen tension (TcPO2) was noted in the group of patients with successful revascularisation of the foot arteries, compared with patients with two below-the-knee vessels at the ankle level with partial foot outflow (p<0.001).11
In 2010, Abdelhamid et al. reported longer-term outcomes following angioplasty of pedal and plantar arteries in 42 CLI cases. Technical success was 88.0% – similar to that reported by Manzi et al., while limb salvage was 81.9% at 2-year follow-up.13 Transdorsal-to-plantar or transplantar-to-dorsal balloon angioplasty for limb salvage in eight CLI patients with diabetes was also reported by Zhu et al. The authors managed to recanalise five out of eight patients (62.5%). Rest pain improved in all cases, wound healing or improvement was noted in two patients and no major amputation was necessary.14
A year later, Alexandrescu et al. published the first results of angiosome-guided infrapopliteal angioplasty with the aim of improving wound healing. In the majority of the patients, additional pedal and plantar artery angioplasty was performed resulting in excellent limb salvage rates.15 The same year, Kawarada et al. published the first study of below-the-ankle stenting. In this retrospective analysis of 40 critical ischaemic limbs (31 patients), balloon-expandable, bare-metal stents were deployed following significant recoil, flow-limiting dissection, abrupt closure or repeat early reocclusion. Technical success was 93.0% and limb salvage was 82.1% at 2-year follow-up. However, the majority of the stents were deformed and two cases of acute or subacute stent occlusion were noted, while reintervention-free rates were disappointing (39.6%, 39.6%, and 35.2%, at 6, 12, and 24 months, respectively).16
Following the unacceptably high clinically significant restenosis rates with bare-metal stents, Katsanos et al. reported outcomes of below-the-ankle angioplasty and bail-out drug-eluting or self-expanding Nitinol stents in a series of 40 limbs in 37 CLI patients. Provisional stenting was used as a bail-out option following suboptimal angioplasty in 45.2% of the cases. Coronary drug-eluting stents (DES) were implanted in 57.9% of the cases, and self-expanding Nitinol stents were implanted in the remaining 42.1%. Despite the fact that half of the DES implanted were deformed or fractured during follow-up, self-expanding stents were associated with significantly higher restenosis and lower primary patency rates compared with balloon angioplasty or DES. The overall binary restenosis rate was 64.1% and repeat intervention-free survival was 93.6% at 1-year follow-up.17 Stent deformation and fracture is common in this specific anatomical area, which can be described as ‘stent non-friendly’.18 Stents (preferably DES) should be reserved for real bail-out cases, such as when the patient is facing amputation.
Palena et al. retrospectively analysed 38 CLI patients who had undergone transmetatarsal arterial access and retrograde recanalisation of the foot and the tibial vessels, resulting in a satisfactory amputation-free survival rate of 81.5% at 1-year follow-up.19
In 2016, in another retrospective single-centre study, Nakama et al. investigated the clinical utility of additional pedal angioplasty in 29 CLI patients and, for the first time, an angiographic criterion for pedal angioplasty was described.20 Specifically, pedal arch angioplasty was performed only if no sufficient wound blush around the target wounds was noted following above-the-ankle, tibial revascularisation. The authors compared outcomes of 14 limbs with additional pedal arch angioplasty and 18 limbs without pedal arch angioplasty as a result of sufficient wound blush. Technical success rate was 93% (13 of 14 patients), and following successful pedal arch angioplasty sufficient wound blush was achieved. Interestingly, despite the fact that limb salvage, amputation-free survival and freedom from reintervention were similar between the two study groups, wound healing (93.0% versus 60.0%; p=0.05) and time to wound healing (86.0 ± 18.7 versus 152.0 ± 60.2 days; p=0.05) were significantly improved in patients who underwent pedal arch angioplasty.
In 2017, the same group published the outcomes of the first large scale multicentre registry. 21 The Retrospective Analysis for the Clinical Impact of Pedal Artery Revascularization Versus Non-Revascularization Strategy for Patients With Critical Limb Ischemia (RENDEZVOUS) retrospective registry investigated a total of 257 CLI patients divided into two groups based on the performance of additional pedal angioplasty (n=140) or not (n=117). Again, wound healing and time to wound healing were significantly improved in the pedal angioplasty group compared with the no pedal angioplasty group (57.5% versus 37.3%; p=0.003 and 211 days versus 365 days; p=0.008, respectively). However, after patient stratification into low-, medium- and high-risk groups according to a delayed wound healing score, adjunctive pedal arch angioplasty was found to improve the rate of wound healing only in the medium-risk population. In the high-risk population, additional pedal arch angioplasty did not contribute to an improvement in wound healing.
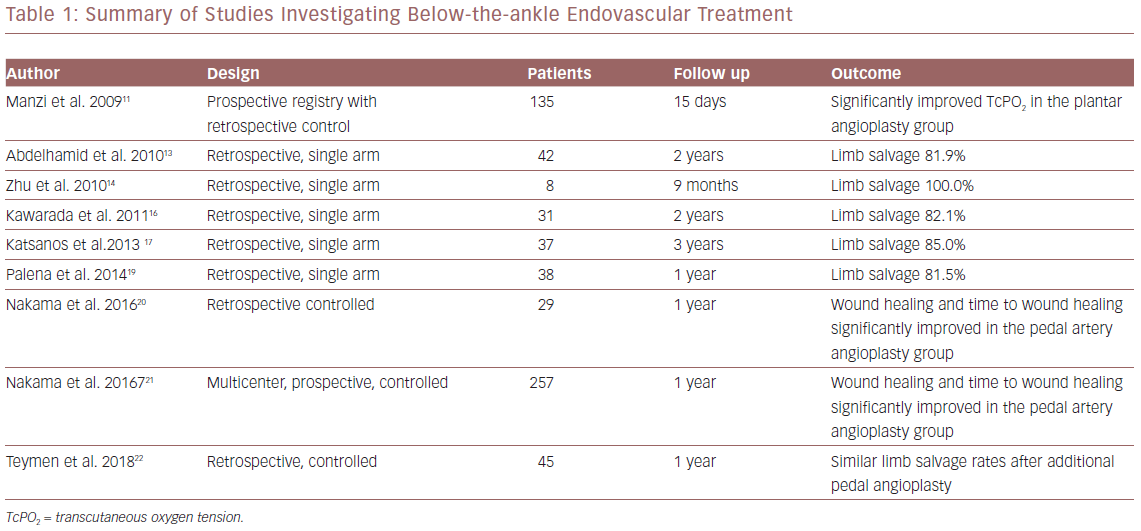
Finally, in 2018 Teymen et al. published the results of a retrospective, single-centre study comparing patients who underwent additional below-the-ankle angioplasty (n=20) or below-the-knee angioplasty only (n=25), using drug-coated balloons.22 Mean lesion length was similar in the two groups (36.40 ± 8.14 mm versus 33.40 ± 7.25 mm in the below-the-ankle and below-the-knee only groups, respectively). Interestingly, the 1-year restenosis rate was low in the below-the-ankle group, marginally missing the level of statistical significance (15.8% versus 47.8%; p=0.059). However, amputation and survival rates were similar between the two groups. All available studies are summarised in Table 1.
Future Perspectives
Below-the-ankle angioplasty is part of everyday clinical practice in experienced vascular centres. Despite the initial positive clinical outcomes for CLI patients with small-vessel outflow disease and poor limb salvage prognosis, data for inframalleolar angioplasty remain limited to single-centre, mainly retrospective case series’ with a small number of patients and only one large, retrospective, multicentre registry. There is no solid evidence demonstrating that additional pedal angioplasty improves limb salvage rates, although there are strong indications that wound healing and time to wound healing are significantly improved in medium-risk patients. Several issues remain to be determined, such as clear indications for pedal angioplasty and the extent of pedal arch reconstruction, as well as the feasibility and effectiveness of various novel endovascular devices, such as drug-coated balloons, drug-infusion catheters, lithoplasty, balloons that minimise dissections and atherectomy devices in the specific anatomical area.
It should be highlighted that although limb salvage remains a clear clinical endpoint, wound healing and, more specifically, time to wound healing, should also be evaluated. Non-healing or slowly-healing ulcers directly affect the patient’s quality of life, creating major economic and social consequences. Novel technologies currently under investigation have enabled assessment of the metabolic activity of the revascularised tissue as well as real-time tissue perfusion imaging to accurately quantify outcomes of tissue reperfusion following revascularisation.23 To address these issues, large, prospective, controlled studies designed to quantify tissue perfusion and wound healing following endovascular treatment are awaited.
References
- Norgren L, Hiatt WR, Dormandy JA, et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg 2007;45:S5–67.
Crossref| PubMed - Dua A, Lee CJ. Epidemiology of peripheral arterial disease and critical limb ischemia. Tech Vasc Interv Radiol 2016;19:91–5.
Crossref| PubMed - Spiliopoulos S, Kitrou P, Katsanos K, Karnabatidis D. Current phase II drugs under investigation for the treatment of limb ischemia. Expert Opin Investig Drugs 2015;24:1447–58.
Crossref| PubMed - Uccioli L, Meloni M, Izzo V, et al. Critical limb ischemia: current challenges and future prospects. Vasc Health Risk Manag 2018;14:63–74.
Crossref| PubMed - Diehm N, Rohrer S, Baumgartner I, et al. Distribution pattern of infrageniculate arterial obstructions in patients with diabetes mellitus and renal insufficiency – implications for revascularization. Vasa 2008;37:265–73.
Crossref| PubMed - Rashid H, Slim H, Zayed H, et al. The impact of arterial pedal arch quality and angiosome revascularization on foot tissue loss healing and infrapopliteal bypass outcome. J Vasc Surg 2013;57:1219–26.
Crossref| PubMed - Toursarkissian B, D’Ayala M, Stefanidis D, et al. Angiographic scoring of vascular occlusive disease in the diabetic foot: relevance to bypass graft patency and limb salvage. J Vasc Surg 2002;35:494–500.
Crossref| PubMed - Soder HK, Manninen HI, Jaakkola P, et al. Prospective trial of infrapopliteal artery balloon angioplasty for critical limb ischemia: angiographic and clinical results. J Vasc Interv Radiol 2000;11:1021–31.
Crossref| PubMed - Schillinger M, Exner M, Mlekusch W, et al. Endovascular revascularization below the knee: 6-month results and predictive value of C-reactive protein level. Radiology 2003;227:419–25.
Crossref| PubMed - Siablis D, Karnabatidis D, Katsanos K, et al. Infrapopliteal application of sirolimus-eluting versus bare metal stents for critical limb ischemia: analysis of long-term angiographic and clinical outcome. J Vasc Interv Radiol 2009;20:1141–50.
Crossref| PubMed - Manzi M, Fusaro M, Ceccacci T, et al. Clinical results of below-the knee intervention using pedal-plantar loop technique for the revascularization of foot arteries. J Cardiovasc Surg (Torino) 2009;50:331–7.
PubMed - Fusaro M, Dalla Paola L, Biondi-Zoccai G. Pedal-plantar loop technique for a challenging below-the-knee chronic total occlusion: a novel approach to percutaneous revascularization in critical lower limb ischemia. J Invasive Cardiol 2007;19:E34–7.
PubMed - Abdelhamid MF, Davies RS, Rai S, et al. Below-the-ankle angioplasty is a feasible and effective intervention for critical leg ischaemia. Eur J Vasc Endovasc Surg 2010;39:762–8.
Crossref| PubMed - Zhu YQ, Zhao JG, Li MH, et al. Retrograde transdorsal-to-plantar or transplantar-to-dorsal intraluminal re-entry following unsuccessful subintimal angioplasty for below-the-ankle arterial occlusion. J Endovasc Ther 2010;17:712–21.
Crossref| PubMed - Alexandrescu V, Vincent G, Azdad K, et al. A reliable approach to diabetic neuroischemic foot wounds: below-the-knee angiosome-oriented angioplasty. J Endovasc Ther 2011;18:376–87.
Crossref| PubMed - Kawarada O, Yokoi Y, Higashimori A, et al. Stent assisted below-the-ankle angioplasty for limb salvage. J Endovasc Ther 2011;18:32–42.
Crossref| PubMed - Katsanos K, Diamantopoulos A, Spiliopoulos S, et al. Below- the-ankle angioplasty and stenting for limb salvage: anatomical considerations and long-term outcomes. Cardiovasc Intervent Radiol 2013;36:926–35.
Crossref| PubMed - Karnabatidis D, Katsanos K, Spiliopoulos S, et al. Incidence, anatomical location, and clinical significance of compressions and fractures in infrapopliteal balloon-expandable metal stents. J Endovasc Ther 2009;16:15–22.
Crossref| PubMed - Palena LM, Brocco E, Manzi M. The clinical utility of below-the-ankle angioplasty using “transmetatarsal artery access” in complex cases of CLI. Catheter Cardiovasc Interv 2014;83:123–9.
Crossref| PubMed - Nakama T, Watanabe N, Kimura T, et al. Clinical implications of additional pedal artery angioplasty in critical limb ischemia patients with infrapopliteal and pedal artery disease. J Endovasc Ther 2016;23:83–91.
Crossref| PubMed - Nakama T, Watanabe N, Haraguchi T, et al. Clinical outcomes of pedal artery angioplasty for patients with ischemic wounds: results from the multicenter RENDEZVOUS Registry. JACC Cardiovasc Interv 2017;10:79–90.
Crossref| PubMed - Teymen B, Akturk S. Comparison of drug eluting balloon angioplasty to infrapopliteal artery critical lesions with or without additional pedal artery angioplasty in patients with diabetes mellitus and critical limb ischemia. J Interv Cardiol 2018;31:400–6.
Crossref| PubMed - Reekers JA, Koelemay MJ, Marquering HA, van Bavel ET. Functional imaging of the foot with perfusion angiography in critical limb ischemia. Cardiovasc Intervent Radiol 2016;39:183–9.
Crossref| PubMed
